Improve Your Revenue Cycle Management
Optimize Your Oracle Health Revenue Cycle for Faster Payments
Revenue Cycle Management involves complex patient accounting, claims, and collections. Delays and inefficiencies can impact your bottom line. Our platform pinpoints exactly where issues occur, guiding you through practical steps to streamline operations, reduce errors, and accelerate cash flow.
Download our pre-configured data template and address common challenges to reach your efficiency goals. Follow our six-step improvement plan and consult the Data Template Guide to transform your operations.
Show detailed description
Unlocking Efficiency in Oracle Health Revenue Cycle Management
The financial health of any healthcare organization hinges on effective Revenue Cycle Management, RCM. Within the intricate ecosystem of Oracle Health Revenue Cycle, managing patient accounting, claims, and collections efficiently is paramount. Inefficiencies here can lead to significant revenue leakage, increased operational costs, and compliance risks. Understanding the end-to-end journey of a billing event, from service initiation to final payment, is crucial for maintaining a healthy cash flow and ensuring timely reimbursement. Process optimization in this critical area isn't just about cutting costs, it's about safeguarding your organization's financial stability and enhancing overall patient satisfaction through seamless administrative processes.
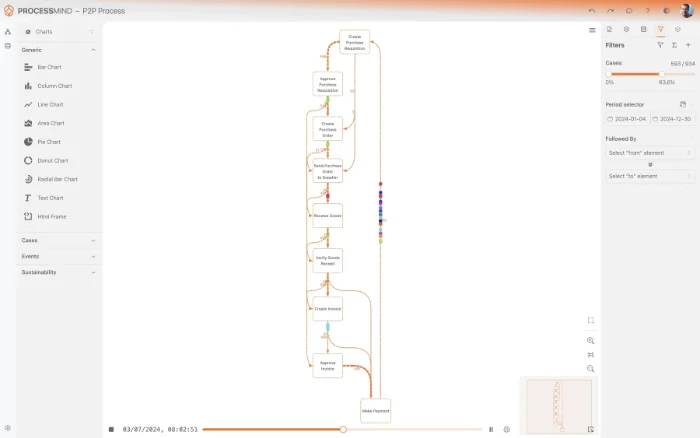
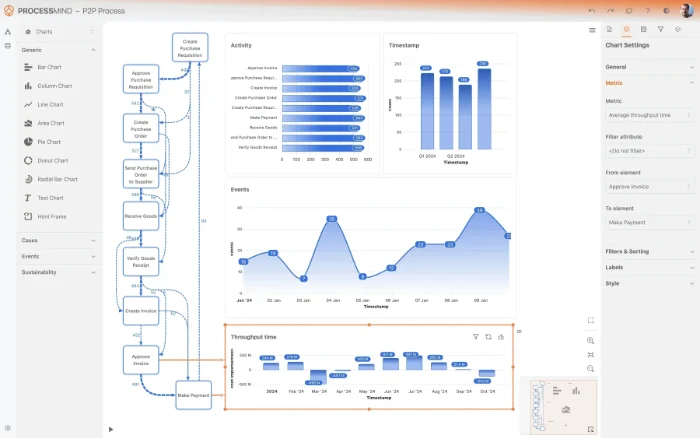
How Process Mining Illuminates Your RCM Journey
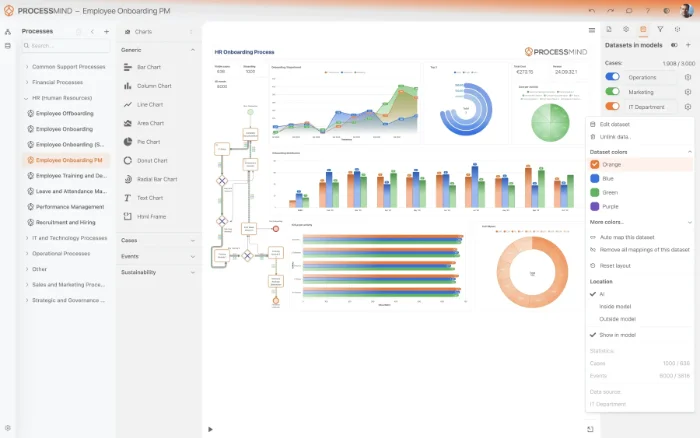
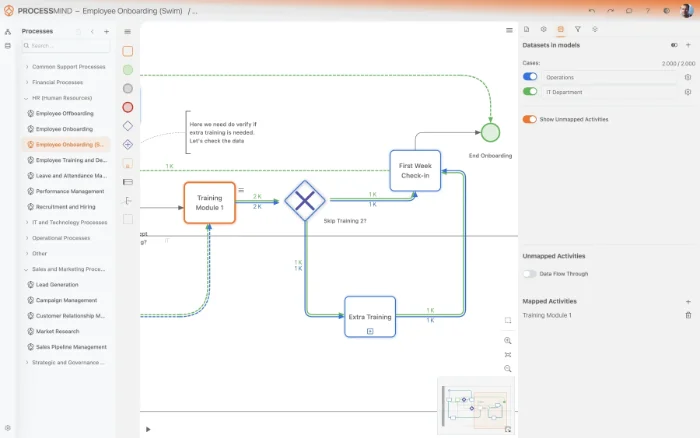
Process mining offers an unparalleled approach to dissecting the complexities of your Oracle Health Revenue Cycle. Instead of relying on assumptions or aggregated reports, this methodology provides a data-driven, X-ray view into the actual path each billing event takes. By leveraging event logs from your Oracle Health system, process mining reconstructs the complete process flow, visualizing every step from service delivery and charge capture to payment posting and account closure. This end-to-end visibility allows you to pinpoint exact bottlenecks, understand the root causes of delays, and identify deviations from your ideal process. You can see precisely where claims get stuck, why payments are delayed, or which disputes prolong the revenue cycle, enabling you to reduce Revenue Cycle Management cycle time effectively. For instance, you might discover that a specific billing department consistently takes longer to generate invoices, or that certain service types frequently lead to payment disputes.
Key Areas for Oracle Health RCM Improvement
With process mining, you gain the actionable insights needed to drive targeted improvements across your Revenue Cycle Management process. Typical areas for optimization include:
- Accelerating Claims Processing: Identify delays in claim submission, tracking, and resubmission, leading to faster reimbursement.
- Optimizing Payment Velocity: Uncover inefficiencies in payment posting and reconciliation, ensuring funds are applied accurately and promptly.
- Enhancing Denials Management: Analyze the root causes of claim denials, allowing you to implement proactive strategies to reduce future rejections and improve first-pass resolution rates.
- Streamlining Charge Capture: Detect gaps or errors in charge entry, ensuring all services provided are accurately billed and minimizing lost revenue.
- Improving Collections Strategies: Evaluate the effectiveness of different collection activities, identifying patterns that lead to quicker resolution of outstanding balances.
- Reducing Manual Interventions: Pinpoint activities that require excessive manual rework or approvals, indicating opportunities for automation or process redesign within Oracle Health.
By focusing on these areas, you move beyond reactive problem-solving to proactive process optimization.
Measurable Outcomes of RCM Process Optimization
Implementing process mining insights in your Oracle Health Revenue Cycle is not just about making processes smoother, it's about achieving tangible, measurable results that directly impact your bottom line. You can expect:
- Increased Cash Flow: By reducing billing errors and accelerating payment cycles, you improve the speed and predictability of your revenue.
- Reduced Operational Costs: Streamlining workflows, automating manual tasks, and minimizing rework directly lowers administrative expenses.
- Decreased Denials and Write-offs: Proactive identification and resolution of issues lead to higher claim acceptance rates and less uncollected revenue.
- Enhanced Compliance: A clearer understanding of process adherence helps ensure your operations meet regulatory requirements and internal policies, mitigating risks.
- Faster Revenue Cycle Cycle Time: Overall reduction in the time it takes for a service to convert into cash, leading to greater financial agility.
- Improved Patient Satisfaction: A smoother, more transparent billing experience contributes positively to the patient journey.
These outcomes empower your organization to achieve a healthier financial standing and dedicate more resources to patient care.
Taking Control of Your Revenue Cycle Management
Improving Revenue Cycle Management in Oracle Health Revenue Cycle doesn't require an army of consultants. This guide provides a structured approach to leverage process mining for powerful insights and actionable steps. By focusing on your actual process data, you gain the clarity needed to make informed decisions, drive efficiency, and transform your financial operations. Start your journey towards a more agile, compliant, and profitable Revenue Cycle Management process today, building a foundation for sustained financial success.
The 6-Step Improvement Path for Revenue Cycle Management
Download Your Template
What to do
Obtain the Excel template designed for Revenue Cycle Management process data. This template provides the correct structure for your Oracle Health Revenue Cycle data.
Why it matters
A structured template ensures data consistency, simplifies mapping, and prepares your information for accurate process analysis, setting a strong foundation.
Expected outcome
An Excel template specific to RCM, ready for your Oracle Health Revenue Cycle data.
WHAT YOU WILL GET
Discover Hidden Efficiencies in Oracle Health RCM
- Visualize your actual RCM process flows.
- Identify precise bottlenecks in patient accounting.
- Pinpoint root causes of claim denials.
- Accelerate cash flow through optimized collections.
TYPICAL OUTCOMES
Achieving Revenue Cycle Excellence
These outcomes illustrate the tangible benefits organizations commonly achieve by applying process mining to their Revenue Cycle Management. By analyzing Oracle Health Revenue Cycle data, particularly around Billing Events, we identify critical inefficiencies, bottlenecks, and opportunities for automation, leading to improved financial performance.
Average reduction in charge capture to invoice time
Process mining reveals bottlenecks in charge capture and invoice generation, enabling organizations to significantly shorten the time from service delivery to billing, improving cash velocity.
Decrease in the overall invoice dispute rate
By pinpointing root causes of disputes, such as incorrect coding or missing documentation, process mining helps reduce the percentage of invoices that lead to costly and time-consuming disputes.
Reduction in average payment posting cycle time
Streamlining the payment posting process through process mining ensures that received payments are quickly and accurately applied to accounts, improving reconciliation and financial reporting.
Increase in end-to-end process conformance
Process mining provides full visibility into process deviations, helping organizations enforce standard operating procedures and regulatory requirements, minimizing compliance risks.
Average reduction in DSO
Optimizing collection strategies and accelerating billing cycles directly translates to a lower Average Days Sales Outstanding, significantly boosting an organization's cash flow.
Results are indicative and may vary based on the unique characteristics of your organization's Revenue Cycle Management processes, the specific configuration of Oracle Health Revenue Cycle, and data completeness. These figures represent typical improvements observed across a range of implementations.
Recommended Data
FAQs
Frequently asked questions
Process mining visualizes your complete RCM process flow, from charge capture to account closure. It helps identify bottlenecks, like slow invoicing or frequent payment disputes, enabling targeted improvements to accelerate cash flow and reduce revenue erosion.
You will primarily need event logs detailing your billing events. This includes a case identifier, typically a Billing Event ID, along with activity names, and corresponding timestamps for each step. This data allows the process mining tool to reconstruct the actual process flow.
Data extraction typically involves querying relevant tables in your Oracle Health database or utilizing existing reporting tools. The goal is to collect event logs in a structured format, usually CSV or a database connection, which can then be fed into the process mining software.
Initial setup, including data extraction and model creation, can range from a few weeks to a couple of months, depending on data complexity and availability. You can often see the main process flows and obvious bottlenecks within the first month after data ingestion.
You can expect to uncover hidden inefficiencies, reduce cycle times for activities like dispute resolution, and identify root causes for issues such as frequent adjustments or re-issuance. This leads to faster payments, improved compliance, and optimized resource allocation in your billing department.
Yes, process mining utilizes dedicated software platforms designed to analyze event logs. While Oracle Health provides the source data, you will need a process mining tool and someone with analytical skills to interpret the results and translate them into actionable insights.
Absolutely. Process mining allows you to visualize every actual process path, comparing them against defined compliance rules and standard operating procedures. This helps quickly identify deviations and non-compliant process instances, enabling proactive correction and risk mitigation.
Process mining is a non-invasive analytical technique. It works by analyzing historical data, so it does not directly interfere with your live RCM operations. The primary effort involves initial data extraction and ongoing data refreshes, which can be automated.
Optimize Your Revenue Cycle for Faster Payments
Eliminate bottlenecks, reduce cycle time by 30%, and boost cash flow.
No credit card required. Set up in minutes.