Improve Your Patient Journey
Optimize Your Patient Journey for Better Care
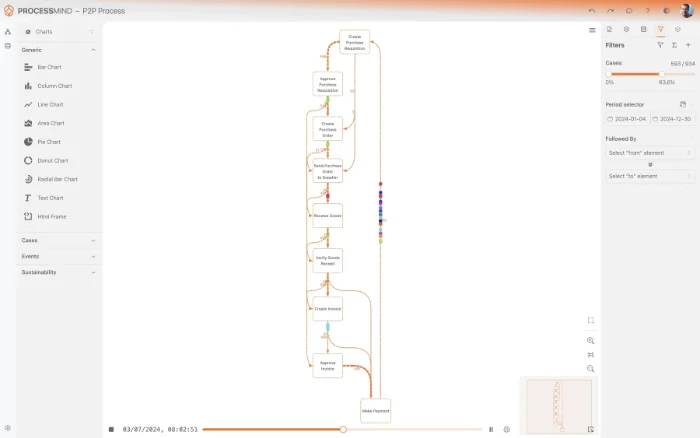
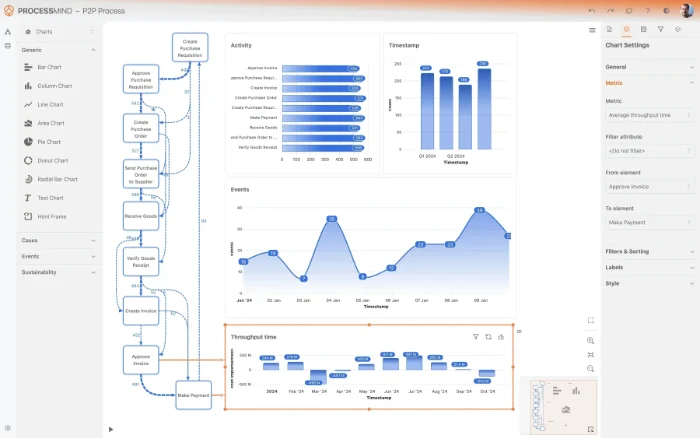
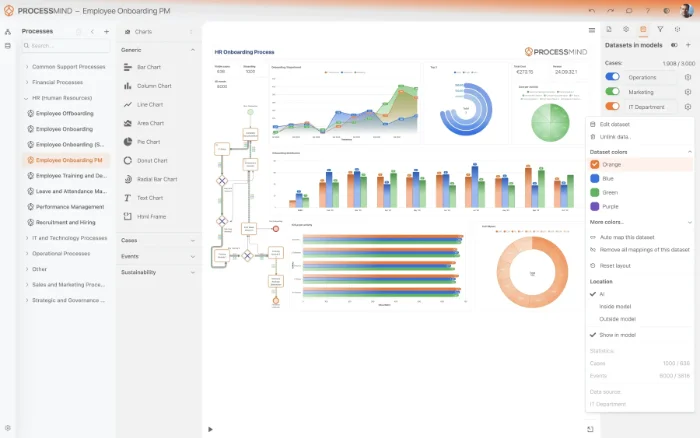
Process mining allows you to uncover hidden bottlenecks and deviations within your workflows by analyzing event logs from your source system. By mapping every Patient Episode, you can identify where delays occur and how to optimize resource utilization. Our platform provides the visibility needed to transform your data into a more streamlined care experience.
Download our pre-configured data template and address common challenges to reach your efficiency goals. Follow our six-step improvement plan and consult the Data Template Guide to transform your operations.
Show detailed description
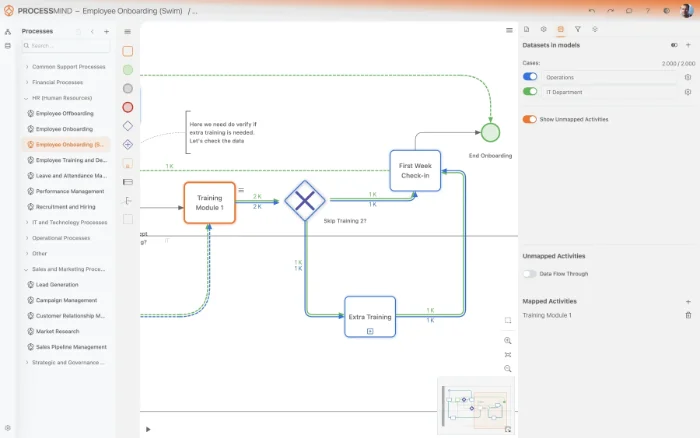
Process mining offers an unprecedented view of the patient journey by stitching together every touchpoint from initial registration to final discharge. By leveraging data directly from your source system, the platform builds a comprehensive map of how patients move through your facilities. This reveals the actual path taken by a patient episode, which often deviates significantly from the standard clinical protocols designed by management. You can see precisely where transitions between departments stall, how clinical documentation lags behind actual care, and where administrative hurdles create friction. This level of transparency allows healthcare administrators to move beyond anecdotal evidence and make decisions based on the granular reality of their daily operations. By visualizing the as-is process, organizations can finally address the root causes of inefficiency that have remained hidden within the silos of different departments.
In many healthcare organizations, bottlenecks are often hidden within complex workflows that span multiple departments. By analyzing your patient journey data, you can uncover exactly where these delays occur, whether they are in the diagnostic phase, during specialist consultations, or within the discharge planning process. These inefficiencies do not just impact patient satisfaction, they also represent significant compliance risks and financial leakage. For example, if your system shows that certain mandatory screenings or administrative steps are being skipped or performed out of sequence, you can intervene before these gaps affect patient safety or reimbursement eligibility. The platform highlights these variances automatically, regardless of the complexity of your current ERP or clinical data architecture. It allows for a deep dive into the cycle times of each stage, providing a clear picture of how long a patient episode remains in each status and where the process deviates from the expected norm.
The ultimate goal of analyzing the patient journey is to ensure that every patient receives the right care at the right time. When you understand the flow of every patient episode, you can optimize resource allocation and staff scheduling to meet actual demand patterns. This data driven approach enables you to identify high performing pathways that lead to shorter stays and better recovery rates, allowing you to replicate those successes across the entire organization. By streamlining the patient journey, you reduce the burden on your clinical staff and create a more seamless experience for the patients themselves. The insights gained from our process mining technology help turn raw data from your source systems into actionable strategies for continuous improvement. By focusing on the entire patient episode, you can move away from departmental optimization and toward a holistic view of care delivery that prioritizes the patient experience.
Getting started with process mining for your patient journey is a straightforward process that does not require a complete overhaul of your technical environment. We provide a comprehensive data template designed to work with the structures found in your existing systems, ensuring that you can map your patient episodes without extensive custom coding. Simply connect your source system to our platform to begin the transformation of your raw event logs into a dynamic, interactive process map. By following our standardized data requirements, you can quickly move from data ingestion to meaningful insight, allowing your team to focus on what matters most, providing exceptional care. Our platform is built to be inclusive of any technical setup, ensuring that every organization can benefit from a transparent view of their patient care delivery. Once your data is connected, you can immediately begin identifying opportunities to reduce lead times, improve throughput, and enhance the overall quality of care.
The 6-Step Patient Journey Improvement Path
Connect and Discover
What to do
Extract patient episode data from your clinical records and map timestamps for registration, triage, and discharge.
Why it matters
Establishing a data foundation allows you to see the real patient flow instead of relying on subjective interviews or manual logs.
Expected outcome
A raw digital footprint of every patient episode across all departments.
WHAT YOU WILL GET
Unlock Hidden Insights into Every Patient Interaction
- Map every step of the real patient journey
- Identify bottlenecks in clinical workflows
- Reduce treatment lead times and wait periods
- Ensure compliance with healthcare protocols
PROVEN OUTCOMES
Optimizing Every Stage of the Patient Episode
Healthcare providers leverage process mining to visualize the complete patient journey, identifying opportunities to remove delays and improve clinical compliance. These outcomes are the result of transforming system data into clear, actionable pathways for better care.
Average reduction in patient stay
Optimizing discharge planning and internal transfers helps minimize unnecessary days in care, which frees up critical bed capacity for new admissions.
Improvement in turnaround time
Identifying bottlenecks between test orders and result delivery allows clinicians to make informed decisions faster, leading to more timely treatment for patients.
Increase in protocol compliance
Visualizing deviations from established clinical pathways ensures patients receive standardized care that aligns with safety and regulatory standards.
Reduction in unplanned returns
Analyzing the discharge process and post-care follow-ups identifies root causes of early returns, leading to better patient health and significant cost savings.
Reduction in initial waiting times
Streamlining the flow from registration to initial assessment reduces waiting room times and ensures patients receive clinical care earlier in their journey.
Efficiency gains in care delivery
Improving resource allocation and reducing the time spent on internal transfers maximizes the use of facilities and decreases the cost per patient episode.
Individual results vary based on process complexity, data quality, and organizational implementation. These figures illustrate the typical efficiency gains observed across similar healthcare environments.
Recommended Data
For customized data recommendations, choose your specific process.
FAQs
Frequently asked questions
Process mining uses event log data from your system to visualize how patients move through your facility. It identifies hidden bottlenecks, such as triage delays or ward transfer lags, providing a data-driven view of patient flow that traditional reporting might miss.
To perform an analysis, you primarily need event logs that include three core components, which are a unique identifier like a Patient Episode, clear activity names, and precise timestamps for each step. Additional attributes like department names or patient demographics can be added to provide deeper context for the analysis.
The technology identifies exactly where the journey stalls, whether patients are waiting for transport, test results, or physician sign-off. By visualizing these friction points, clinical managers can implement targeted changes to shorten cycles and increase bed availability.
Data security is a top priority, and the setup typically involves de-identifying sensitive information before the data is analyzed. You can filter out protected health information while retaining the sequence of events necessary to optimize clinical operations and comply with healthcare regulations.
Initial findings are often available within four to six weeks once the data extraction from your source system is finalized. The first few weeks focus on data mapping and validation, after which the software provides ongoing visibility into operational efficiency.
Standard reports provide static metrics like average wait times, while process mining visualizes the actual movement and loops between different events. It reveals hidden paths, rework, and deviations that traditional business intelligence tools often miss, uncovering the root causes of inefficiency.
Process mining is non-intrusive and works by analyzing the digital footprints already created during the normal course of patient care. It captures the process as it currently exists without requiring staff to change how they document activities in the source system.
By analyzing the full patient journey, the tool can find correlations between specific treatment paths and unplanned readmissions. You might discover that patients who experience rushed discharge planning or skip specific follow-up steps are more likely to return, allowing for better standardization of care protocols.
Data is generally pulled from the underlying reporting databases or audit logs of the source system using standard queries or automated pipelines. This process focuses on capturing the digital footprint of a patient episode, which is then transformed into a structured format for analysis.
Start Optimizing Your Patient Journey Today
Identify care bottlenecks and improve outcomes in minutes
No credit card required. Fast setup.