Improve Your Claims Processing
Optimize Claims Processing in Guidewire ClaimCenter for Swift Resolution
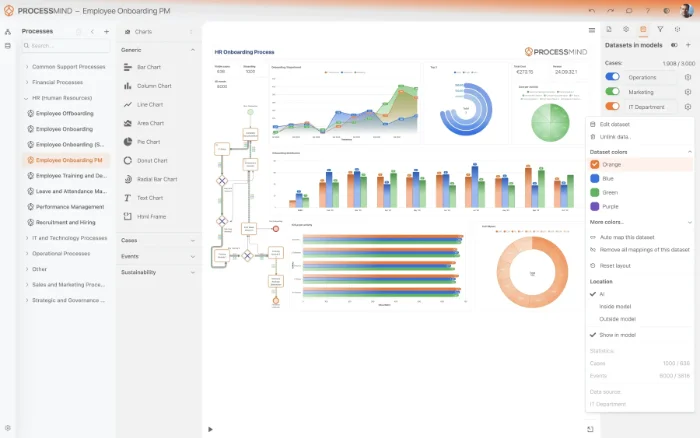
Our platform helps you uncover hidden inefficiencies and process variations within your operations. Easily pinpoint bottlenecks, understand deviations from desired paths, and identify root causes of delays. By providing data-driven insights, we enable you to streamline workflows, reduce operational costs, and improve overall process performance.
Download our pre-configured data template and address common challenges to reach your efficiency goals. Follow our six-step improvement plan and consult the Data Template Guide to transform your operations.
Show detailed description
Why Optimizing Claims Processing is Crucial for Your Business
Claims processing stands at the heart of any property & casualty (P&C) insurance company, directly impacting customer satisfaction, operational costs, and regulatory compliance. In a competitive landscape, the efficiency and transparency of your claims handling can be a significant differentiator. However, the inherent complexity of managing diverse claim types, intricate policy details, and numerous external interactions often leads to delays, inefficiencies, and rising costs. Operating within a robust system like Guidewire ClaimCenter provides a strong foundation, but even with industry-leading technology, the actual execution of processes can diverge from the ideal. Unseen bottlenecks, manual workarounds, and non-standard procedures can accumulate, resulting in longer cycle times, increased administrative overhead, and frustrated policyholders. Understanding the true 'as-is' state of your Claims Processing in Guidewire ClaimCenter is the first step towards transforming it from a potential cost center into a streamlined, customer-centric operation.
How Process Mining Illuminates Your Claims Workflows
Process mining offers a powerful, data-driven lens to meticulously analyze your Claims Processing directly from the event logs within Guidewire ClaimCenter. Unlike traditional business intelligence or manual process mapping, process mining leverages actual system data – such as every 'Claim Submitted', 'Initial Review Performed', 'Payment Issued' activity, along with their timestamps and associated claim IDs – to reconstruct the entire claims journey with pinpoint accuracy. This provides an unbiased, objective view of how claims truly flow, rather than how they are assumed to flow.
Specifically, for Claims Processing within Guidewire ClaimCenter, process mining enables you to:
- Identify Bottlenecks with Precision: Pinpoint exact stages or activities where claims experience undue delays, whether it's awaiting an 'Investigation Completed' status or bogged down in the 'Payment Authorization' queue. You'll see which specific adjuster or department contributes to the longest waiting times.
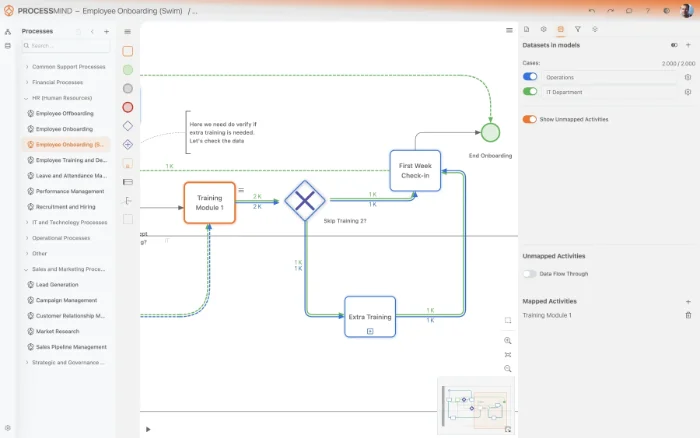
- Uncover Process Deviations: Visualize all variant paths claims take, differentiating between the most common, efficient routes and those that involve excessive rework, multiple approvals, or unnecessary steps. This helps highlight non-standard operations that increase costs and cycle times.
- Analyze Root Causes of Delays: Delve deeper into the factors contributing to extended cycle times, such as the volume of 'Additional Information Requested' activities, the number of handovers between adjusters, or specific claim types that consistently face delays.
- Monitor Compliance Automatically: Verify adherence to internal policies and regulatory requirements by comparing the actual process flow against predefined models, flagging any deviations that could pose compliance risks or increase potential fraud.
- Measure Cycle Times Accurately: Gain precise measurements of end-to-end claim cycle times, as well as the duration of individual sub-processes, allowing you to benchmark performance and track improvements over time.
By leveraging the rich data from Guidewire ClaimCenter, process mining provides the evidence needed to move beyond guesswork and implement targeted, impactful process optimization.
Key Areas for Claims Processing Improvement
With the detailed insights gained from process mining your Guidewire ClaimCenter data, you can strategically target several critical areas for improvement:
- Streamline Workflows: Eliminate redundant steps, consolidate activities, and optimize the sequence of tasks. For instance, identify if 'Initial Review' and 'Loss Assessed' can be better integrated or automated for certain claim types.
- Reduce Rework and Exceptions: Analyze why claims frequently re-enter certain stages, like multiple 'Investigation Started' activities, or why 'Claim Decision Made' leads to a 'Re-evaluation Requested'. Addressing these exceptions reduces manual effort and speeds up resolution.
- Optimize Resource Allocation: Understand how different adjusters or teams handle similar claims, identifying best practices and areas where training or workload rebalancing could mitigate resource bottlenecks.
- Enhance Communication & Handovers: Identify where handovers between departments or external parties (e.g., medical providers, repair shops) introduce delays and implement strategies to smooth these transitions.
- Improve Compliance & Risk Management: Proactively identify patterns indicative of non-compliance or potential fraud, allowing for earlier intervention and risk mitigation within your Guidewire environment.
Expected Outcomes of Process Optimization
Implementing process improvements identified through process mining on your Guidewire ClaimCenter data translates into tangible benefits that directly impact your bottom line and customer experience:
- Significantly Reduced Cycle Times: Achieve faster claim resolution, leading to quicker payments and a superior experience for your policyholders. This directly addresses the goal of how to reduce Claims Processing cycle time.
- Lower Operational Costs: Decrease manual effort, minimize rework, and reduce potential penalties arising from non-compliance, leading to substantial cost savings.
- Increased Efficiency and Throughput: Process more claims with the same or fewer resources, optimizing the utilization of your Guidewire ClaimCenter system and personnel.
- Enhanced Policyholder Satisfaction: Deliver a more transparent, predictable, and fair claims experience, fostering loyalty and positive brand perception.
- Stronger Compliance and Risk Posture: Proactively detect and mitigate deviations from internal policies and external regulations, reducing financial and reputational risks.
- Data-Driven Decision Making: Empower your teams with factual insights to make informed decisions about process changes, technology investments, and resource planning.
Getting Started with Your Claims Processing Transformation
Embarking on the journey to optimize your Claims Processing in Guidewire ClaimCenter doesn't require extensive prior process mining expertise. Our approach guides you through connecting your Guidewire data, analyzing your processes, and identifying actionable improvements. By leveraging these insights, you can move towards a more efficient, compliant, and customer-centric claims operation, turning data into a powerful competitive advantage. Start uncovering the hidden potential within your Claims Processing today.
The 6-Step Improvement Path for Claims Processing
Download the Template
What to do
Obtain the ProcessMind data template tailored for Claims Processing from Guidewire ClaimCenter to ensure proper structuring of your claim data for analysis.
Why it matters
Using the right template prevents data quality issues and simplifies the subsequent analysis, setting a strong foundation for accurate insights.
Expected outcome
A structured Excel template ready to guide the extraction of your Guidewire ClaimCenter data.
Export Your Claim Data
What to do
Extract 3-6 months of historical claims data from your Guidewire ClaimCenter system, populating the downloaded ProcessMind template with real operational data.
Why it matters
Comprehensive historical data allows for robust process analysis, uncovering recurring patterns and performance trends over a meaningful period.
Expected outcome
A completed ProcessMind template filled with 3-6 months of your Guidewire ClaimCenter claims data.
Upload Your Dataset
What to do
Securely upload your populated ProcessMind data template containing Guidewire ClaimCenter claims data to the ProcessMind platform for automated processing.
Why it matters
Quickly transforming raw data into a visual process map accelerates time-to-insight, allowing you to focus on analysis rather than data preparation.
Expected outcome
Your Guidewire claims data successfully uploaded and ready for automatic process visualization and analysis in ProcessMind.
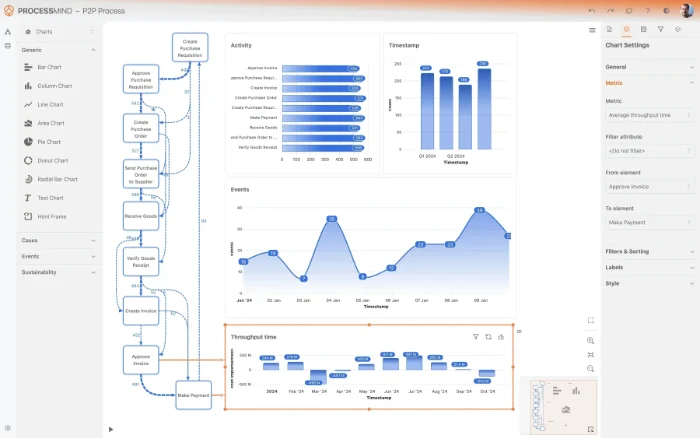
Analyze Your Claims Process
What to do
Explore the automatically generated dashboards and insights within ProcessMind, leveraging AI-driven recommendations to identify bottlenecks in your claims workflow.
Why it matters
Understanding the true end-to-end claims journey reveals inefficiencies, compliance gaps, and areas where Guidewire ClaimCenter usage can be optimized.
Expected outcome
A clear understanding of your Claims Processing workflow, pinpointing specific areas for improvement and optimization.
Implement Claims Improvements
What to do
Prioritize and implement the identified opportunities to streamline your claims processing, making targeted changes within Guidewire ClaimCenter operations or policies.
Why it matters
Translating insights into action directly improves operational efficiency, reduces cycle times, and enhances policyholder satisfaction in claims resolution.
Expected outcome
Strategic changes actively deployed within your Guidewire ClaimCenter environment, addressing identified process inefficiencies.
Monitor Claims Performance
What to do
Periodically re-upload fresh data from Guidewire ClaimCenter to ProcessMind to continuously track progress and measure the impact of your implemented improvements.
Why it matters
Continuous monitoring ensures that improvements are sustained, new issues are quickly identified, and the claims process remains optimized over time.
Expected outcome
Quantifiable KPI improvements in claims processing, demonstrating the tangible benefits and ongoing optimization of your workflow.
WHAT YOU WILL GET
Visualize Your Claims Process for Swiftness
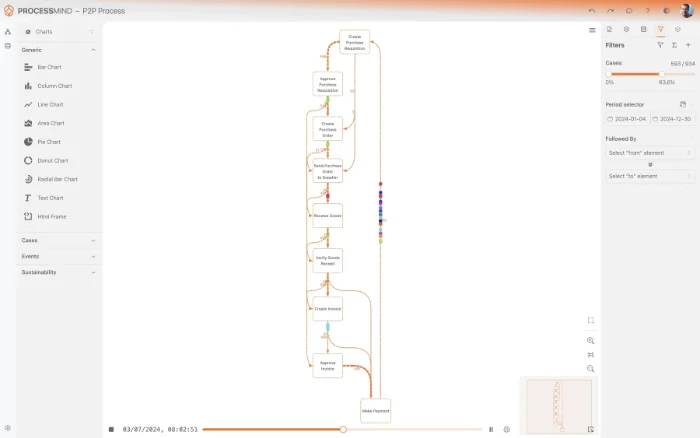
- Visualize actual claims process flows
- Pinpoint exact bottlenecks and delays
- Compare claims performance variants
- Track compliance and resolution times
TYPICAL OUTCOMES
Transforming Claims Processing with Measurable Results
These outcomes represent the tangible improvements organizations typically achieve by applying process mining to their claims processing, identifying bottlenecks, and streamlining workflows within systems like Guidewire ClaimCenter. They highlight how data-driven insights lead to significant operational efficiencies and enhanced claimant experiences.
Average reduction in end-to-end time
Streamline the entire claims process from submission to closure, significantly reducing the time taken for customers to receive their settlement. This improves customer satisfaction and operational efficiency.
Decrease in claim re-processing and rejections
Identify root causes of claim rework and rejections to minimize repetitive tasks and errors. This leads to higher first-pass resolution rates and lower operational costs.
Higher adherence to regulatory standards
Ensure claims are processed according to defined policies and regulatory requirements by identifying and rectifying deviations. This reduces audit risks and ensures consistent service delivery.
Reduction in manual effort and processing costs
Pinpoint inefficient steps and repetitive manual activities to automate or eliminate them, leading to significant savings in operational expenses. This frees up adjusters for more complex tasks.
Shorter cycle time for required data
Optimize the process of requesting and receiving additional information from claimants or third parties. This reduces bottlenecks and accelerates overall claim resolution.
Higher percentage of claims meeting targets
Achieve better performance against internal and external service level agreements by identifying and addressing delays. This leads to improved customer satisfaction and operational reliability.
Results vary based on process complexity, data quality, and specific implementation scope. These figures represent typical improvements observed across various claims processing implementations.
Recommended Data
FAQs
Frequently asked questions
Process mining analyzes event logs from ClaimCenter to visualize the actual claims journey. It uncovers bottlenecks, rework loops, and deviations from the standard path. This helps accelerate settlements, reduce rejections, and ensure regulatory compliance.
You typically need event logs containing a Case ID (Claim ID), Activity Name (e.g., "Claim Opened," "Investigation Started," "Payment Authorized"), and Timestamp for each activity. Additional attributes like adjuster ID, claim type, or status changes enhance analysis. This data helps reconstruct the precise sequence of events.
Data extraction can often be done via standard reporting tools, SQL queries directly on the database (if allowed), or through ClaimCenter's API/integration layer. The goal is to obtain event logs in a structured format. Collaboration with your IT team and understanding ClaimCenter's data model is crucial for accurate extraction.
You can expect significant improvements such as reduced claim settlement times, fewer rejections due to identified rework, and enhanced adherence to regulatory guidelines. Process mining helps standardize processes, optimize adjuster workload, and ultimately lower operational costs per claim.
No, process mining goes beyond traditional reporting or business intelligence. While reporting shows "what happened," process mining reveals "how and why" it happened by reconstructing the actual process flow from event data. It discovers process variations, compliance gaps, and root causes of inefficiencies that standard reports often miss.
Initial data extraction and model setup can typically take a few weeks, depending on data availability and complexity. Once the initial model is built, you can often see actionable insights and identify major bottlenecks within 4-8 weeks. Continuous monitoring then provides ongoing optimization opportunities.
Beyond access to ClaimCenter's event data, you'll need a process mining software platform, which can be cloud-based or on-premises. This platform requires sufficient processing power and storage for your historical data. Integration capabilities for data ingestion are also key.
Yes, process mining is highly effective for compliance. It can automatically detect deviations from mandated process steps or service level agreements (SLAs). By visualizing every case's journey, it highlights instances where regulations might have been overlooked, reducing risks of penalties and ensuring consistent adherence.
Accelerate Claims Processing, Resolve Cases Faster Now
Eliminate backlogs, prevent fraud, and target 70% straight-through processing.
No credit card required, setup in just minutes.