Improve Your Claims Processing
Optimize Claims Processing in Sapiens ClaimsPro for Faster Resolution
Claims processing can often suffer from delays, compliance issues, and inconsistent resolutions. Our platform helps you uncover hidden inefficiencies and identify root causes of bottlenecks. Streamline your entire claims workflow to enhance operational efficiency and boost customer satisfaction.
Download our pre-configured data template and address common challenges to reach your efficiency goals. Follow our six-step improvement plan and consult the Data Template Guide to transform your operations.
Show detailed description
Why Optimizing Claims Processing is Critical for Your Business
Claims Processing is the lifeblood of any insurance operation, directly impacting customer satisfaction, financial performance, and regulatory compliance. Inefficient claims handling, even within robust systems like Sapiens ClaimsPro, can lead to substantial financial losses through delayed payments, increased operational costs, and unnecessary reserves. Furthermore, slow or inconsistent claims resolution can severely damage your reputation, erode customer trust, and lead to policyholder churn. The inherent complexity of managing diverse claim types, navigating regulatory requirements, and coordinating multiple stakeholders means that manual oversight often misses subtle yet significant inefficiencies. Understanding the true flow and identifying the specific points of friction within your Claims Processing operations, powered by Sapiens ClaimsPro data, is not just beneficial—it’s essential for sustained business success and competitive advantage.
How Process Mining Illuminates Claims Workflows in Sapiens ClaimsPro
Your Sapiens ClaimsPro system captures a wealth of transactional data, logging every activity, event, and status change for each claim. Process mining takes this raw event data – from "Claim Submitted" to "Payment Issued" – and visually reconstructs the actual end-to-end journey of every single claim. Unlike traditional analytics that show what should happen or summary statistics, process mining reveals what does happen. This means you can:
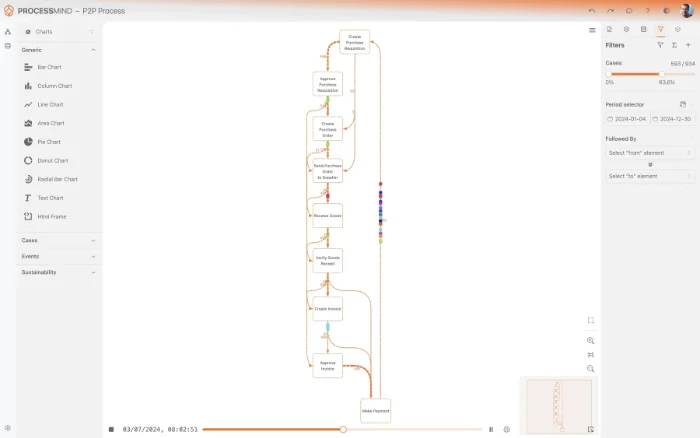
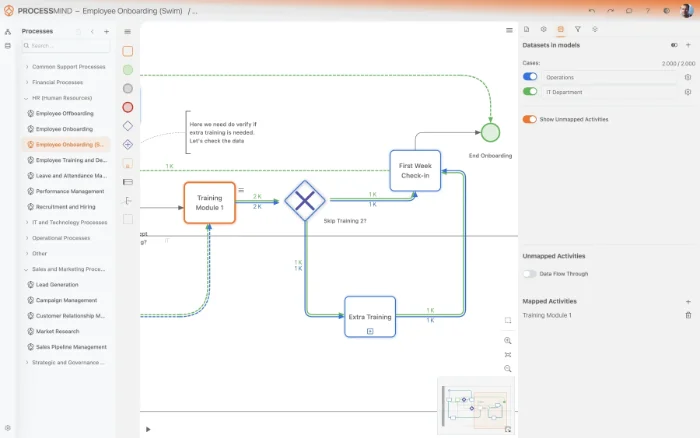
- Visualize Real Workflows: See all executed paths, even the deviations from the standard process, identifying where claims get stuck or take unexpected detours within Sapiens ClaimsPro.
- Pinpoint Bottlenecks: Precisely identify activities or handoffs that cause delays. Is the bottleneck in "Initial Review Performed," "Investigation Completed," or "Payment Authorized"? Process mining shows you the exact waiting times and queues.
- Analyze Rework and Loops: Detect instances where claims repeatedly cycle between statuses, such as multiple "Additional Information Requested" events, indicating process friction or unclear communication.
- Quantify Cycle Times: Measure the precise duration of each process step and the overall end-to-end claim resolution time, offering a factual basis for performance improvement initiatives. This helps you understand how to reduce Claims Processing cycle time effectively.
By leveraging the detailed event logs from your Sapiens ClaimsPro system, process mining provides an X-ray view into your claims operations, offering unparalleled transparency and actionable insights.
Uncovering Key Improvement Areas within Your Claims Operations
With a clear understanding of your claims process derived from process mining, you can target specific areas for significant improvement:
- Streamlining Adherence to SLAs: Identify claims that consistently breach service level agreements and investigate the root causes, whether it’s resource allocation, approval delays, or external dependencies.
- Optimizing Resource Allocation: Analyze adjuster workloads, handoff times, and task assignments to ensure an even distribution and minimize idle time or burnout. This could involve re-evaluating team structures or automation opportunities within Sapiens ClaimsPro.
- Enhancing Compliance and Audit Readiness: Automatically detect non-compliant process paths or skipped mandatory steps, ensuring that every claim adheres to regulatory requirements and internal policies. This proactive identification is crucial for risk management.
- Reducing Manual Touchpoints and Rework: Pinpoint repetitive manual tasks or frequent re-dos (e.g., repeatedly requesting the same information) that can be automated, simplified, or better supported by Sapiens ClaimsPro features.
- Identifying Best Practices: Compare the performance of different process variants or teams to identify successful strategies that can be scaled across the organization, leading to more consistent and efficient Claims Processing.
Tangible Outcomes: Elevating Your Claims Performance
Implementing process-mining-driven improvements for your Claims Processing in Sapiens ClaimsPro leads to concrete and measurable benefits across your organization:
- Significantly Reduced Cycle Times: Expedite claim resolution, leading to faster payouts and higher policyholder satisfaction. This directly addresses the goal of how to reduce Claims Processing cycle time.
- Lower Operational Costs: By eliminating bottlenecks, reducing rework, and optimizing resource utilization, you can achieve substantial savings in operational expenditure and adjuster time.
- Boosted Compliance and Reduced Risk: Proactively identify and rectify deviations from regulatory and internal standards, mitigating financial penalties and reputational damage.
- Enhanced Customer Experience: Deliver consistent, transparent, and quicker claim resolutions, fostering trust and loyalty among your policyholders.
- Data-Driven Decision Making: Empower your management with factual, objective insights into process performance, enabling informed decisions for strategic improvements and system enhancements within Sapiens ClaimsPro.
These outcomes translate into a stronger competitive position, improved financial health, and a more agile, customer-centric organization.
Getting Started with Claims Processing Optimization
Transforming your Claims Processing through process optimization doesn't require a complete overhaul or extensive technical expertise. By connecting to your Sapiens ClaimsPro data, process mining tools can quickly deliver the deep insights you need to understand, analyze, and dramatically improve your claims workflows. Start leveraging the power of your existing data to uncover hidden efficiencies and drive tangible improvements across your Claims Processing operations today.
The 6-Step Improvement Path for Claims Processing
Download the Template
What to do
Access the pre-built ProcessMind Excel template specifically designed for Claims Processing. This template provides the correct structure for your Sapiens ClaimsPro data.
Why it matters
Starting with the right data structure ensures compatibility and accuracy, laying a solid foundation for meaningful process analysis.
Expected outcome
A ready-to-use Excel template tailored for efficient claims data collection.
Export Your Claims Data
What to do
Extract 3-6 months of historical claims processing data directly from your Sapiens ClaimsPro system. Populate the downloaded template with your real operational data.
Why it matters
Comprehensive historical data provides a realistic view of your current claims process, enabling accurate identification of patterns and inefficiencies.
Expected outcome
A populated Excel template containing a rich dataset of your recent claims processing activities.
Upload Your Claims Dataset
What to do
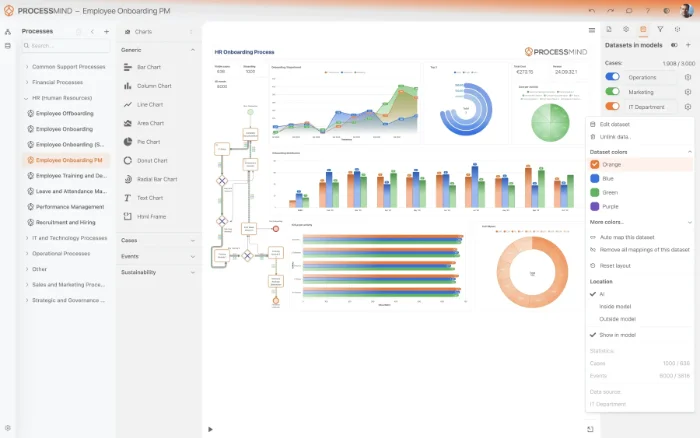
Securely upload your completed claims data template to ProcessMind. Our platform automatically processes and prepares your data for analysis.
Why it matters
A secure and efficient upload ensures your sensitive claims data is handled safely, quickly transforming raw data into an analyzable format.
Expected outcome
Your Sapiens ClaimsPro data successfully ingested and ready for process mining analysis.
Analyze Claims Process
What to do
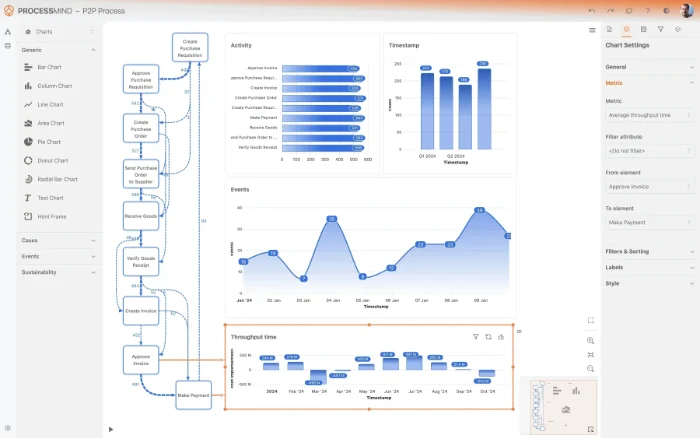
Explore the auto-generated dashboards and interactive process maps within ProcessMind. Leverage AI-driven recommendations to pinpoint bottlenecks and non-compliance.
Why it matters
Visual insights and intelligent suggestions reveal the true performance of your claims handling, highlighting areas for immediate efficiency gains and risk reduction.
Expected outcome
A clear understanding of your claims process variations, bottlenecks, compliance issues, and actionable improvement insights.
Implement Key Improvements
What to do
Prioritize the identified improvement opportunities from ProcessMind's analysis. Develop and execute concrete action plans to address inefficiencies in Sapiens ClaimsPro.
Why it matters
Acting on data-backed insights directly translates into tangible operational benefits, such as reduced cycle times and lower processing costs.
Expected outcome
Implemented changes within your Sapiens ClaimsPro workflow leading to a more efficient and compliant claims process.
Monitor Process Performance
What to do
Periodically re-upload fresh claims data from Sapiens ClaimsPro to ProcessMind to continuously track the impact of your improvements.
Why it matters
Ongoing monitoring ensures sustained efficiency gains and allows for proactive adjustments, maintaining optimal performance over time.
Expected outcome
Continuous tracking of claims processing KPIs, demonstrating measurable improvements and sustained operational excellence.
YOUR CLAIMS INSIGHTS
See Your Claims Journey, Discover Key Bottlenecks
- Visualize actual claims processing flows
- Pinpoint delay root causes in Sapiens ClaimsPro
- Identify compliance breaches and rework loops
- Quantify impact of process changes on claims
TYPICAL OUTCOMES
Transformative Outcomes in Claims Processing
By applying process mining to your Sapiens ClaimsPro data, organizations uncover critical bottlenecks and inefficiencies in their claims workflows. These outcomes represent typical improvements observed in key performance areas.
Average reduction in end-to-end processing
Identify and eliminate bottlenecks to significantly reduce the time from claim submission to closure, enhancing customer experience.
Decrease in claims requiring additional info
Pinpoint root causes of rework loops and additional information requests, leading to a more streamlined and efficient initial claim processing.
Higher percentage of claims meeting deadlines
Ensure more claims are resolved within target dates by optimizing process paths and proactively addressing potential delays, boosting customer trust.
Reduction in process deviations
Enforce consistent claim handling by identifying and correcting non-standard process paths, improving predictability and reducing compliance risks.
Average percentage reduction in operational costs
Optimize resource allocation and eliminate unnecessary activities to significantly decrease the average operational cost associated with processing each claim.
Individual results may vary based on your specific process complexity, data integrity, and operational context. The figures presented illustrate common gains realized through our solutions.
Recommended Data
FAQs
Frequently asked questions
Process mining provides a data-driven X-ray of your actual claims journey within Sapiens ClaimsPro. It uncovers hidden bottlenecks, deviations from standard paths, and sources of rework, allowing for precise optimization. This leads to faster resolution times and increased operational efficiency.
You primarily need event log data containing a unique Case ID (e.g., Claim ID), an Activity Name (what action occurred), and a Timestamp (when the action happened). Sapiens ClaimsPro usually stores this in its database, and extracting these three core elements is fundamental for mapping your process.
Expect significant improvements such as reduced claim resolution times, fewer re-submissions, and better adherence to regulatory compliance. Process mining helps optimize resource allocation and can lead to a lower average cost per claim, increasing overall transparency and efficiency.
Extracting data from Sapiens ClaimsPro usually involves standard database queries to access its underlying tables. While initial data cleaning and transformation might be necessary to fit the "Case ID, Activity, Timestamp" format, it's generally a manageable task for someone familiar with SQL or reporting tools.
Yes, process mining excels at identifying non-compliant claim handling paths and deviations from established rules. It visualizes every process instance against defined regulations, allowing you to proactively detect and correct instances where policies are not followed within Sapiens ClaimsPro.
Process mining complements existing reports by providing a dynamic, visual understanding of the flow of work, rather than just static metrics. It answers "why" certain KPIs are observed by showing the actual process variations, offering deeper diagnostic insights beyond traditional dashboards.
After successful data extraction and transformation, initial process models and insights can often be generated within days or a few weeks. The speed depends on data availability and the complexity of the claims process being analyzed.
Basic data analysis skills are beneficial, along with familiarity with data structures, potentially SQL for data extraction. Many modern process mining tools are designed with user-friendly interfaces, minimizing the need for advanced technical expertise for ongoing analysis once data is configured.
Absolutely. By identifying bottlenecks and workload imbalances, process mining clearly shows where resources are over or underutilized in your claims department. This enables data-driven decisions to redistribute tasks, improve staffing levels, and reduce processing delays caused by resource constraints.
Accelerate Claims Processing, Eliminate Backlogs Today
Join companies achieving 70% straight-through processing and rapid settlements.
No credit card required, set up in minutes.