Improve Your Patient Journey
Optimize MEDITECH Patient Journey for Enhanced Efficiency
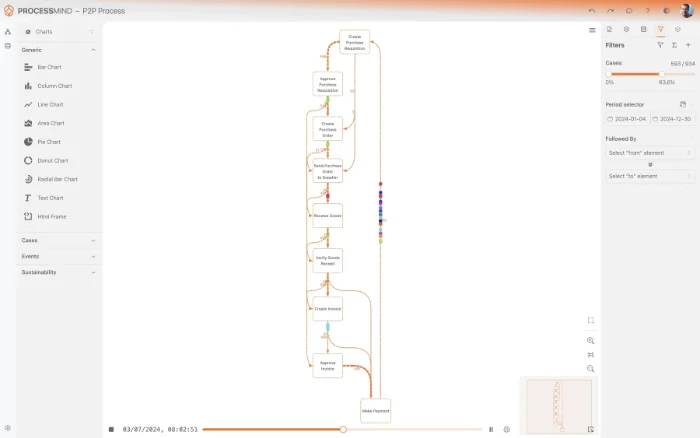
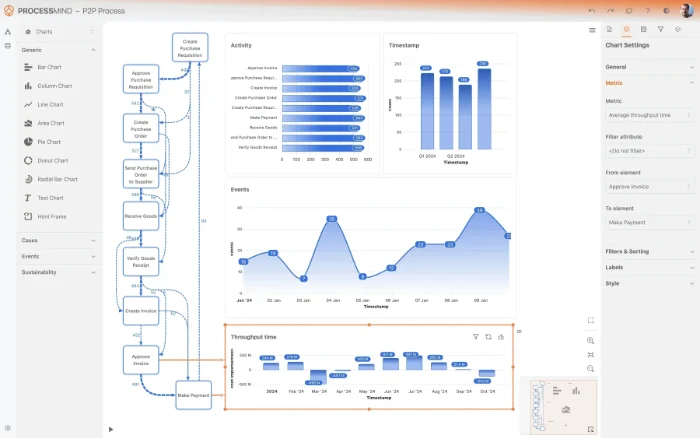
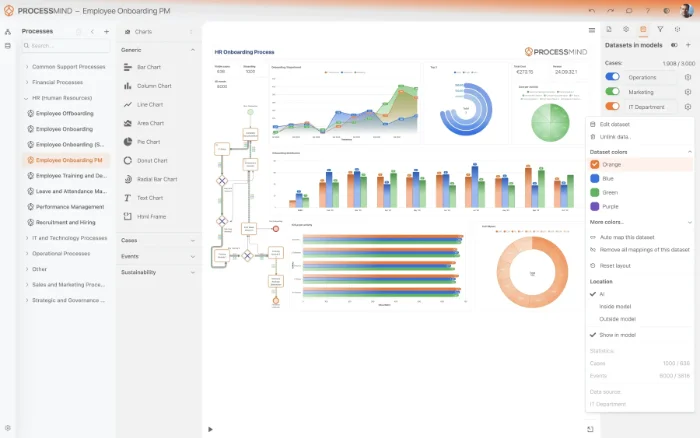
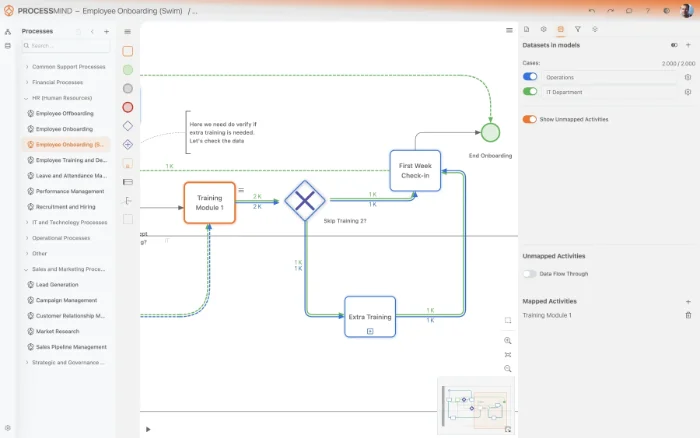
Process mining uncovers hidden bottlenecks and variations that disrupt clinical efficiency. Our platform helps you visualize the flow of care to pinpoint where delays occur and how resources are allocated. By identifying these friction points, you can streamline operations and enhance the overall experience for everyone involved.
Download our pre-configured data template and address common challenges to reach your efficiency goals. Follow our six-step improvement plan and consult the Data Template Guide to transform your operations.
Show detailed description
The Value of Optimizing the Patient Journey
The patient journey is the most complex process within any healthcare organization. In the MEDITECH environment, this journey spans across multiple modules and departments, making it difficult to maintain a unified view of efficiency. Optimizing the patient journey is not just about moving people through the system faster, it is about ensuring that every step adds value to clinical outcomes and patient safety. When flow is stagnant, it creates a domino effect that impacts bed capacity, emergency department wait times, and clinician burnout. By focusing on process optimization, healthcare leaders can ensure that the right care is delivered at the right time, reducing the unnecessary overhead that often plagues large medical institutions.
From a business perspective, the cost of inefficiency is staggering. Delayed discharges lead to lost revenue through bed blocking, while extended wait times in the emergency department can lead to patients leaving without being seen. Process mining provides the necessary lens to view these operational challenges as manageable data points. By understanding the flow within MEDITECH Expanse, organizations can transition from a reactive state of managing crises to a proactive culture of continuous improvement. This shift is essential for maintaining a competitive edge and meeting the high standards of modern value-based care models.
How Process Mining Transforms Care Delivery
Process mining serves as a diagnostic tool for your hospital operations. By extracting event data directly from MEDITECH, you can reconstruct exactly how patients move through your facility in real time. Instead of relying on anecdotal evidence or time-consuming manual audits, you gain a transparent, data-driven view of every interaction. This visibility allows leadership to see where patients deviate from established clinical protocols or where administrative delays, such as insurance verification or transportation wait times, stall the healing process.
The unique advantage of process mining in a MEDITECH environment is its ability to connect disparate data points. It links the registration in the ambulatory setting to the acute care triage and the eventual discharge and follow-up. This end-to-end visibility is crucial for identifying the true root causes of bottlenecks. For instance, a delay in the emergency department might actually be caused by a slow discharge process in the surgical ward. Process mining allows you to trace these dependencies across the entire organization, providing a single source of truth for process performance.
Identifying and Addressing Clinical Bottlenecks
One of the primary areas for improvement in the patient journey is the transition between departments. For example, the time between a physician ordering a diagnostic test in the MEDITECH Expanse platform and the technician performing that test can vary significantly depending on the time of day or the specific department involved. Process mining helps you isolate these specific handoff points. By analyzing the time spent in each state, you can identify if delays are caused by staffing shortages, equipment availability, or communication gaps within the MEDITECH interface itself.
Another critical area is the discharge planning process. Often, the medical decision to discharge happens much earlier than the patient's physical exit from the building. Identifying the lag between the discharge order and the actual departure can unlock significant bed capacity. Process mining reveals the specific activities, such as waiting for final lab results or coordinating with post-acute facilities, that extend the length of stay. By streamlining these final steps, hospitals can improve throughput and ensure that beds are available for incoming patients who need them most.
Measurable Benefits and Clinical Outcomes
The outcomes of these optimization initiatives are measured in both clinical quality and financial sustainability. Reducing the overall cycle time of a patient episode directly correlates to a lower average length of stay. For hospitals, this means the ability to treat more patients without increasing the physical footprint of the facility. Furthermore, streamlining the journey reduces the likelihood of medical errors associated with long wait times or rushed transitions between care teams. When the process is smooth, clinicians can focus more on the patient and less on navigating administrative hurdles.
Compliance and adherence to medical protocols also see a significant boost. Process mining can automatically flag instances where required documentation, such as a sepsis screening or a fall risk assessment, was bypassed or delayed. This automated monitoring ensures that every patient receives a standardized level of care, regardless of which department they are in or which clinician is attending to them. Over time, these incremental improvements lead to higher patient satisfaction scores and better overall clinical reputations.
Getting Started with Your Optimization Strategy
To begin your journey toward a more efficient hospital, you must first define the boundaries of your analysis. Starting with the patient episode as your primary case identifier allows you to see the full picture from the initial point of contact to the final follow-up. By utilizing specialized templates designed to work with the MEDITECH data structure, you can quickly move from data extraction to actionable insights. The goal is to create a living map of your processes that evolves as your hospital grows.
You are encouraged to start with a specific department or high-volume diagnosis to prove the value of the approach. Once you have identified and cleared the bottlenecks in one area, the methodology can be scaled across the entire enterprise. This proactive approach to process management transforms your MEDITECH EHR from a simple record-keeping system into a powerful engine for operational excellence and superior patient care.
The 6-Step Improvement Path for Patient Journey
Download the Template
What to do
Access the standardized Excel template designed for MEDITECH Patient Journey and review the required structure for clinical encounter data.
Why it matters
Starting with a structured format ensures that patient milestones like triage and discharge are captured correctly for deep process analysis.
Expected outcome
A ready-to-use template for organizing your clinical data.
YOUR CLINICAL INSIGHTS
Uncover Every Delay in Your MEDITECH Patient Flow
- Map complete MEDITECH clinical pathways
- Pinpoint triage and discharge bottlenecks
- Reduce patient wait times systematically
- Optimize resource usage across departments
PROVEN OUTCOMES
Enhancing the Patient Experience
By analyzing patient episodes within MEDITECH systems, organizations identify critical bottlenecks and streamline care delivery to improve clinical performance. These benchmarks reflect the typical efficiency gains achieved through targeted process mining initiatives.
Efficiency in end to end episodes
Optimizing discharge planning and internal transfers reduces the total time patients spend in the facility, which frees up critical bed capacity for new arrivals.
Standardized clinical pathways
Process mining identifies deviations from gold standard protocols, ensuring patients receive consistent care based on their specific primary diagnosis.
Lab and imaging turnaround
Accelerating the time between test orders and performance allows clinicians to make informed decisions and start treatments sooner, improving patient outcomes.
Quality of discharge planning
Analyzing patient journeys helps identify root causes of early readmissions, leading to more robust follow up care and discharge protocols.
Initial assessment throughput
Reducing the gap between registration and initial assessment improves patient safety and optimizes emergency department resource allocation during peak times.
Resource utilization efficiency
Streamlining internal transfers and discharge lead times maximizes the use of existing facilities and reduces the overall cost per patient episode.
Individual results vary based on clinical process complexity and data quality. These figures represent typical improvements observed across healthcare implementations.
Recommended Data
FAQs
Frequently asked questions
Process mining utilizes the timestamped event logs already stored within your MEDITECH system to create a visual map of the actual patient flow. By using the Patient Episode as a unique identifier, the software reconstructs every step from admission to discharge, highlighting where the real process deviates from the intended clinical pathway.
To perform an effective analysis, you need a dataset containing three core components: a unique case ID like the Patient Episode, an activity name for each event, and a precise timestamp. Most hospitals extract this information from the MEDITECH audit trails or transaction logs where clinical and administrative actions are recorded.
Yes, process mining specifically targets bottlenecks in the triage and diagnostic phases by measuring the exact duration between every milestone. By visualizing these delays, administrators can identify whether lags are caused by specialist consultation wait times or resource shortages in specific departments, allowing for data driven staffing adjustments.
Initial findings are typically available within four to six weeks once the data extraction process from MEDITECH is finalized. The first few weeks focus on data mapping to ensure the Patient Episode sequences are accurately captured, after which the software can provide ongoing monitoring of clinical efficiency.
While standard MEDITECH reports provide static metrics like average length of stay, process mining visualizes the actual movement and loops between hospital events. It reveals the hidden paths, rework, and deviations that traditional business intelligence tools often miss, allowing you to see the root causes of inefficiency.
Data security is maintained by anonymizing the Patient Episode identifiers before the data is analyzed by the mining software. This process ensures that the focus remains on operational flow and timing while fully protecting individual patient identities according to regulatory standards.
Process mining compares the actual patient journey against your hospital’s established protocols to find any variations in care. By highlighting where clinical teams skip steps or introduce unplanned transfers, the system provides a clear picture of how well the organization is standardizing treatment plans.
The main requirement is the ability to query the underlying MEDITECH database or export audit logs into structured files like CSV or Parquet. Most organizations utilize an existing data warehouse or an ETL process to gather the required event logs before feeding them into the process mining platform.
Optimize Your Patient Journey and Reduce Delays Now
Reduce cycle times by 30 percent and improve hospital efficiency
No credit card required. Start in minutes.